How to Get Off Prozac Safely available in Amazon. Click here for paperback $12.55 Click here for eBook $7.25.
Read How to Get Off Prozac Safely for free on this website.
How to Get Off Prozac Safely
There is Hope. There is a Solution.
__________
By James Harper
All rights reserved. No part of this book may be reproduced or transmitted in any form or by any means without written permission from the author.
Printed in USA
Dedication
To my mother, I thank you from the bottom of my heart.
As a child you gave me a safe space to just be a child and allowed me to stumble and learn from my mistakes. As an adult you encouraged me to keep looking for new answers.
With your passing you have helped me learn value in each moment. Thank you and you are missed.
To all of you that have helped along the way, your assistance has been invaluable.
Author contact: Jim@theroadback.org
Introduction
AFTER TWENTY-SIX YEARS of research, assisting tens of thousands of people to get off their psychotropic medication, this book is the final and closing chapter of the development of How to Get Off Taper Prozac Safely. Not to say there will not be future advancements in a Prozac withdrawal program, but the foundation needed for a Prozac withdrawal program and health program is now firmly in place. The success rate of people now using this program is higher than ever imagined, the basic causes of Prozac withdrawal symptoms and the human health decline have now been discovered, and the solution is backed by scientific evidence.
This Prozac withdrawal book is written mainly for the patient, or individual wanting to get off Prozac or to simply rebuild or maintain good health after taking Prozac.
If you have tried to withdrawal Prozac in the past and suffered, have found this book in the middle of your Prozac withdrawal or quit Prozac cold turkey, you may have a little more work to do than most, but the success will still be there. With the advancements in How to Get Off Prozac Safely, your path to recovery and achieving well-being—perhaps for the first time in years—can now be attained within a relatively short period.
If you are seeking to improve your overall health, there is usually no need to have patience when you use the program, it works rather quickly. Many of us are just accustomed to feeling how we feel, and we may have lost track of how good we can feel when the body and mind work as a unique team. By doing a few basic things, we can reverse much of what is happening inside of our body and that reversal usually equates to a better attitude in life and a major quality of life improvement.
I want to acknowledge the many people, from the four corners of Earth and all walks of life, who have successfully changed their life while using this program. Their perseverance and feedback have helped advance this program to today’s high degree of success.
And I applaud you, opening this book for the first time, for your courage and resolve to change your life and get yourself back as your reward.
I understand the apprehension you may feel about deciding to come off Prozac, especially if you have tried to do so before and failed, or if you have heard horror stories of others who have tried to come off Prozac.
Further, I understand the questions you might be asking at this point:
- Will I experience mental or physical pain while on this program?
- Will I have other side effects while on this program?
- Will the Prozac side effects get worse before they get better?
- Will my depression get worse during this program?
- Will my anxiety levels increase?
You may have many other questions in addition to those above, but most importantly you should know that How to Taper Prozac can be virtually side effect free. The testament to this, as you will see throughout the book, is that people just like you start to feel better, mentally and physically, sometimes from day one.
You have two options when using this program. You can use the supplements that are recommended or just reduce the Prozac slowly. Jim Harper strongly urges you to include the supplements during the taper.
Why supplements? In 1999, when this withdrawal method was first introduced Jim Harper did not recommend supplements. This was when the reduction of 10% of the original dosage was used for antidepressants, antipsychotics and ADHD medication and a 5% taper if reducing a benzodiazepine. You will see these reduction amounts as the standard now for every drug withdrawal program. Jim also introduced the slow and gradual method for tapering.
During 1999 and 2000, over 1 million people read Jim’s website, and hundreds of thousands used his tapering approach. The results led Jim to believe there had to be a much better way to taper these drugs and began looking at specific supplements. With Prozac prescriptions written quite often in those days, a high percentage of people Jim assisted off their medication were taking Prozac.
What were the results that made Jim look for other solutions?
Fifty percent of the people could taper off their medication by tapering gradually and slowly and by using the 10% or 5% reduction method. The medical community viewed these results as a major breakthrough in tapering a psychotropic medication. The underlying story told a different story altogether.
Of the 50% that made it off their medication, 5% made it off their drug with ease and were able to remain off the drug. However, the other 95% suffered their way through the taper and eventually went back on the medication to get relief from the lingering withdrawal side effects.
Jim Harper would not accept these results as a success.
In 2000, some promises of a better taper method were seen using a whey protein powder that is manufactured to increase a substance called glutathione. Glutathione is the body’s master antioxidant and has several functions to remove toxins from the body. Using this approach increased the success rate of the program by 25%. A great improvement but still far from ideal.
In 2003, another breakthrough came for Jim Harper. A very high percentage of the people tapering Prozac would experience a withdrawal symptom call “brain zaps” during the taper. This is a very debilitating sensation, described as a sudden electrical jolt that runs from the base of the neck up into the head. It is often brought on when a person moves their eyes from side to side or up and down. The Prozac induced brain zaps caused most people to stop their Prozac taper and just go back higher on the Prozac for relief and never attempt to taper Prozac again.
We will not go into the science of how the solution was discovered in this book but provide the solution. Omega 3 fish oil high in EPA is the solution. How much you take and when you take the omega 3 is important as well. Over the years, Jim refined the use of omega 3 to; the best type of fish to use in the oil, when and how much to take. This resulted in using less fish oil as well for the desired results.
In 2004, Jim started a DNA testing company with the idea that our individual DNA held promise in creating an even more successful Prozac withdrawal program. Initially, Jim tested how the medications affect our DNA, and the role DNA played in the metabolism speed of the drugs. Once again, great results came from this research and you will now find in the description of virtually all medications, which DNA metabolism route the drug takes to breakdown and most importantly, which people should or should not use certain medications if their DNA is a certain way.
As great as this information was, it still did not help with tapering Prozac. It only showed why some people could take Prozac and do fine on it and taper it without any problem.
Next, Jim began looking at nutritional supplements, DNA, and tapering. Near the end of 2004, Jim formulated his first supplements that were designed specifically to assist in psychotropic medication withdrawal. Jim sent several bottles to a physician he had been in contact with for several years so he could use them with a group of patients. These patients had been on their psychotropic medication for several years and had not been able to taper of the drug.
All the patients tapered off their medication and did exceptionally well during the taper. All were able to remain off their medication and no original symptoms returned.
Jumping ahead to 2010, Jim discovered a gene that is disrupted when taking any psychotropic medication. The next major breakthrough in tapering followed. Reduce the activation of this gene and withdrawal symptoms fade away and fade away quickly. Over the 15 years since this discovery, Jim has continued his research and the success rate of tapering with his method is still the best in the health community.
This was a short story for you, so you know why Jim recommends specific supplements during the taper. If you choose not to use them, Jim still provides in this book how to taper each type of medication and what to watch out for along your journey.
Life is defined as: the quality that distinguishes a vital and functional being from a dead body or inanimate matter (Webster’s Dictionary). Per the definition of life, you are vital. We need you and humankind needs you. The positive changes you can bring to others are beyond imagination. Life can be grand, life can be fulfilling; you, changing your life and having “reach” return will absolutely affect others in your environment.
Reach can return with your children, spouse, work or activities you have been putting off for years that you have always wanted to do, or to do once again.
Remember and hold the following close to your heart as you travel this journey:
- You Can Change.
- You Can Change How You Feel.
- You Can Be a Positive Influence for Others.
- You Can Make It
My best to all of you on this journey,
James Harper
Chapter 1
Tapering Prozac
Tapering the Prozac, with or without using supplements, is the same. There is an exception to this, and it is imperative to mention.
With you taking Prozac, you will likely need to take omega 3 fish oil. No way around this. When withdrawing from Prozac you will likely develop what is known as “brain Zaps.” These are electrical type jolts that tend to start in the upper neck area and run up into the skull. Moving your eyes to the side or up and down can make the brain zaps start or become worse. Get an omega 3 fish oil that is higher in EPA than DHA or go to www.ngscart.com and look for the Omega 3 Supreme.
You should take 1 softgel in the morning and 1 softgel at noon. You can adjust the omega 3 around to match what works best for you. See the chapter Using Supplements for more detail on using omega 3 to stop the brain zaps.
Prozac Withdrawal Timeline
The timeline for reducing Prozac was established by this program in 1999. You should only reduce Prozac to the next lower dosage if you are feeling very stable on the last reduction. Only reduce the Prozac again if you are feeling very well.
Only reduce Prozac every 2 weeks. It is very fine to wait longer before reducing the Prozac again. Wait until you are feeling stable at the new reduced dosage before you reduce Prozac again.
I will say this repeatedly in this book, Slow and steady wins this race. Do not taper the Prozac sooner than 2 full weeks since the last reduction.
You should reduce the Prozac by no more than 10% of the original dosage.
You do this by getting the Prozac compounded at the pharmacy. Get a 30 day supply each time you compound a new dosage. This way, if you need to stay at that dosage for more than 14 days, you have extra.
If the 10% reduction is too much, compound the Prozac to a 50% reduction. Again, slow and steady wins this race.
If you are reducing the Prozac by 10% reductions and suffering withdrawal still, this would definitely be the time to use the supplements during the Prozac withdrawal process.
Never skip days taking the Prozac when tapering.
Continue taking the Prozac at the same time each day.
Do not quit smoking or start a diet when you are tapering Prozac.
Avoid major life changes while tapering Prozac.
Chapter 2
Prozac Withdrawal Symptoms
This chapter lists many possible side effects experienced from Prozac, or when trying to withdraw from Prozac.
You may know from experience that a single withdrawal side effect can be horrifying. And if you, or anyone you know, have ever had a bad withdrawal experience you would probably rather sign up for open-heart surgery without anesthesia than suffer those side effects again. And for this very reason, many people who have contacted The Road Back are gun shy at the very thought of withdrawing from Prozac. Before The Road Back, you were faced with a quandary: suffer the side effects of Prozac or gut it out and suffer the side effects of withdrawal.
One thing to keep in mind while doing this program or with any inpatient program you might enroll in, if you have a bad day and feel out of sorts, have a headache, ache or a pain, do not sleep well etc., these feelings or symptoms may not be withdrawal. We all have bad days from time to time and how you feel out of the blue can be quite normal. This can be difficult when you have had insomnia for months and begin to sleep better and then out of the blue you have a difficult night sleeping. If the insomnia lasts for more than 3 nights then something needs to be done, but an occasional restless night or sleepless night is common.
This past year we had a person call us and she described how she has had a headache for the past 4 days and how it came out of nowhere. She was ½ way off her medication and doing very well and she felt this was a withdrawal side effect and wanted to know what to do. After a little communication and looking for changes that might have taken place, we found out her best friend had died unexpectedly the day before the headaches started. This might seem easy to spot as a reason for the headaches, but when you are in the middle of withdrawal and you have suffered extreme side effects in the past, it can be easy to lose track and worry about the slightest changes in how you feel.
As you read through the list of potential Prozac side effects in this chapter, do keep in mind these emotional and physical conditions existed long before the first Prozac was manufactured. We are only dealing with drug-induced side effects with this program.
This program helps to eliminate these worries and concerns by reducing the side effects of withdrawal, so that you can come off Prozac smoothly and easily.
The following list is broken down into categories, covering the various areas of the body, such as the nervous system, lymph system, emotional and mental symptoms and so forth. These categories will make it easier for you to find the part of the body or system that you are interested in or want to know more about.
In this list, you will find many physical ailments and complaints, as well as emotional or mental symptoms that people experience every day because of a specific medical condition. These symptoms and ailments may be the reason that you started using a drug, or conversely, these drugs may be causing the negative symptoms you are experiencing now.
This unknown catches almost everyone, doctor and patient alike, off guard. So, the question that needs to be answered for you to proceed with this program is: Are you dealing with a physical condition that needs to be treated medically or with a by-product symptom of the drug(s) you are taking?
Getting Your Doctor’s Approval
Because of the overload and damage potentially caused by Prozac, your body in general, and your immune system in particular, are in a weakened condition, and can thus leave you open to infections and disease. On the other hand, you may be taking prescription medications for actual physical conditions, which could be contra-indicated or need to be closely monitored in terms of doing this program. These could include blood thinners and heart medication, as well as clotting agents.
For these reasons, consult your doctor before starting any part of this program to sort out, or discover and correctly determine whether you are a candidate for this program.
After you have ruled out any real medical problem, you will know that if any strange symptoms begin during this program, you are most likely experiencing something caused by Prozac. Such will be true for both emotional and physical symptoms.
The following list does not include all possible side effects from Prozac; this book would need thousands of pages if this were undertaken. Using the Freedom of Information Act, I received all side effects associated with Prozac during clinical trials. That list alone is long enough to make this book double the size if they are included. The side effects in this chapter are the most common.
Highlight or make a mark by existing symptoms you currently have in the list below.
Dry Mouth – Less moisture in the mouth than is usual.
Increased Sweating – A large quantity of perspiration that is medically caused.
Allergy – Extreme sensitivity of body tissues triggered by substances in the air, drugs, or foods causing a variety of reactions such as sneezing, itching, asthma, hay fever, skin rashes, nausea and/or vomiting.
Asthenia – A physically weak condition.
Chest Pains – Severe discomfort in the chest caused by not enough oxygen going to the heart because of blood vessel narrowing or spasms.
Chills – Appearing pale while cold and shivering. Sometimes accompanied by fever.
Edema of Extremities – Abnormal swelling of body tissue caused by the collection of fluid.
Fall – Suddenly losing a normal standing upright position.
Fatigue – Loss of normal strength thus not able to do usual physical and mental activities.
Fever – Abnormally high body temperature, normal being 98.6 degrees Fahrenheit or 37 degrees Centigrade. Fever is a symptom of disease or disorder in the body. The body is affected by feeling hot, chilled, sweaty, weak and exhausted. If the fever goes too high or lasts too long, death can result.
Hot Flashes – Brief, abnormal enlargement of blood vessels that causes a sudden heat sensation over the entire body. Sometimes experienced by menopausal women.
Influenza (Flu)-like Symptoms – Demonstrating irritation of the respiratory tract (organs of breathing) such as a cold, sudden fever, aches and pains, as well as feeling weak and seeking bed rest, which is similar to having the flu.
Leg Pain – A hurtful sensation in the legs caused by excessive stimulation of the nerve endings in the legs, resulting in extreme discomfort.
Malaise – The somewhat unclear feeling of discomfort when a person starts to feel sick.
Pain in Limb – Sudden, sharp and uncontrolled leg or arm discomfort.
Syncope – A short period of light-headedness or unconsciousness (black- out) also known as fainting, caused by lack of oxygen to the brain because of an interruption in blood flow to the brain.
Tightness of Chest – Mild or sharp discomfort, tightness or pressure in the chest area (anywhere between the throat and belly). The causes can be mild or seriously life-threatening because they include the heart, lungs and surrounding muscles.
CARDIOVASCULAR
(INVOLVING THE HEART AND THE BLOOD VESSELS)
Palpitation – Unusual and abnormal heartbeat that is sometimes irregular, but rapid, and forceful thumping or fluttering. It can be brought on by shock, excitement, exertion or medical stimulants. A person is normally unaware of his/her heartbeat.
Hypertension – High blood pressure, a symptom of disease in the blood vessels leading away from the heart. Hypertension is known as the “silent killer.” The symptoms are usually not obvious; however, it can lead to damage to the heart, brain, kidneys and eyes, and can even lead to stroke and kidney failure.
Bradycardia – The heart rate is slowed from around 72 beats per minute, which is normal, to below 60 beats per minute in an adult.
Tachycardia – The heart rate speeds up to above 100 beats per minute in an adult. Normal adult heart rate is 72 beats per minute.
ECG Abnormal – A test called an electrocardiogram (ECG) records the activity of the heart by measuring heartbeats as well as the position and size of the heart’s four chambers. An ECG also measures whether there is damage to the heart and the effects of drugs or mechanical devices like a heart pacemaker. When the test is abnormal this means one or more of the following are present: heart disease, defects, beating too fast or too slow, disease of the blood vessels leading from the heart or the heart valves, and/or a past or impending heart attack.
Flushing – Skin all over the body turns red.
Varicose Veins – Unusually swollen veins near the surface of the skin that sometimes appear twisted and knotted but always enlarged. They are called hemorrhoids when appearing around the rectum. The cause is attributed to hereditary weakness in the veins aggravated by obesity, pregnancy, pressure from standing, aging, etc. Severe cases may develop swelling in the legs, ankles and feet, eczema and/or ulcers in the affected areas.
GASTROINTESTINAL
Abdominal Cramp/Pain – Sudden, severe, uncontrollable and painful shortening and thickening of the muscles in the belly. The belly includes the stomach, as well as the intestines, liver, kidneys, pancreas, spleen, gall bladder and urinary bladder.
Belching – Noisy release of gas from the stomach through the mouth.
Bloating – Swelling of the belly caused by excessive intestinal gas.
Constipation – Difficulty in having a bowel movement where the material in the bowels is hard due to a lack of exercise, fluid intake, or roughage in the diet or due to certain drugs.
Diarrhea – Unusually frequent and excessive runny bowel movements that may result in severe dehydration and shock.
Dyspepsia/Indigestion – The discomfort one may experience after eating. It can be heartburn, gas, nausea, a bellyache or bloating.
Flatulence – More gas than normal in the digestive organs.
Gagging – Involuntary choking and/or involuntary vomiting.
Gastritis – A severe irritation of the mucus lining of the stomach, either short in duration or lasting for a long period of time.
Gastroenteritis – A condition in which the membranes of the stomach and intestines are irritated.
Gastrointestinal Hemorrhage – Excessive internal bleeding in the stomach and intestines.
Gastro Esophageal Reflux – A continuous state where stomach juices flow back into the throat causing acid indigestion and heartburn and possibly injury to the throat.
Heartburn – A burning pain around the breastbone caused by stomach juices flowing back up into the throat.
Hemorrhoids – Small rounded purplish swollen veins that bleed, itch or are painful and appear around the anus.
Increased Stool Frequency – see “Diarrhea.”
Indigestion – Inability to properly consume and absorb food in the digestive tract, causing constipation, nausea, stomachache, gas, swollen belly, pain and general discomfort or sickness.
Nausea – Stomach irritation with a queasy sensation like motion sickness and a feeling that one is going to vomit.
Polyposis Gastric – Tumors that grow on stems in the lining of the stomach, which usually become cancerous.
Swallowing Difficulty – A feeling that food is stuck in the throat or upper chest area and won’t go down, making it
difficult to swallow.
Toothache – Pain in a tooth above and below the gum line.
Vomiting – Involuntarily throwing up the contents of the stomach, usually accompanied by a nauseated, sick feeling just prior to doing so.
HEMIC & LYMPHATIC
(INVOLVING THE BLOOD AND THE CLEAR FLUIDS IN THE TISSUES THAT CONTAIN WHITE BLOOD CELLS)
Anemia – A condition in which the blood is no longer carrying enough oxygen, so the person looks pale and easily gets dizzy, weak and tired. More severely, a person can end up with an abnormal heart, as well as breathing and digestive difficulties.
Bruise – Damage to the skin resulting in a purple-green- yellow skin coloration that is caused by breaking of the blood vessels in the area without breaking the surface of the skin.
Nosebleed – Blood loss from the nose.
Hematoma – Broken blood vessels that cause a swelling in an area on the body.
Lymphadenopathy Cervical – The lymph nodes in the neck, part of the body’s immune system, become swollen and enlarged by reacting to the presence of a drug. The swelling is the result of the white blood cells multiplying to fight the invasion of the drug.
METABOLIC & NUTRITIONAL
(ENERGY AND HEALTH)
Arthralgia – Sudden sharp nerve pain in one or more joints.
Arthropathy – Joint disease or abnormal joints.
Arthritis – Painfully inflamed and swollen joints. The reddened and swollen condition is brought on by a serious injury or shock to the body either from physical or emotional causes.
Back Discomfort – Severe physical distress in the area from the neck to the pelvis along the backbone.
Bilirubin Increased – Bilirubin is a waste product of the breakdown of old blood cells. Bilirubin is sent to the liver to be made water-soluble so it can be eliminated from the body through emptying the bladder. A drug can interfere with or damage this normal liver function, creating liver disease.
Decreased Weight – Uncontrolled and measured loss of heaviness or weight.
Gout – A severe arthritis condition that is caused by the dumping of a waste product called uric acid into the tissues and joints. It can worsen and cause the body to develop a deformity after going through stages of pain, inflammation, severe tenderness and stiffness.
Hepatic Enzymes Increased – An increase in the amount of paired liver proteins that regulate liver processes causing a condition in which the liver functions abnormally.
Hypercholesterolemia – Too much cholesterol in the blood cells.
Hyperglycemia – An unhealthy amount of sugar in the blood.
Increased Weight – A concentration and storage of fat in the body accumulating over a period of time caused by unhealthy eating patterns, a lack of physical activity, or an inability to process food correctly, which can predispose the body to many disorders and diseases.
Jaw Pain – Pain due to irritation and swelling of the nerves associated with the mouth area where it opens and closes just in front of the ear. Some of the symptoms are pain when chewing, headaches, loss of balance, stuffy ears or ringing in the ears and teeth grinding.
Jaw Stiffness – The result of squeezing and grinding the teeth while asleep that can cause teeth to deteriorate, as well as the muscles and joints of the jaw.
Joint Stiffness – A loss of free motion and easy flexibility.
Muscle Cramp – When muscles contract uncontrollably without warning and do not relax. The muscles of any body organs can cramp.
Muscle Stiffness – The tightening of muscles makes it difficult to bend.
Muscle Weakness – Loss of physical strength.
Myalgia – A general widespread pain and tenderness of the muscles.
Thirst – A strong, unnatural craving for moisture/water in the mouth and throat.
NERVOUS SYSTEM (SENSORY CHANNELS)
Carpal Tunnel Syndrome – A pinched nerve in the wrist that causes pain, tingling, and numbing.
Coordination Abnormal – A lack of normal, harmonious interaction of the parts of the body when it is in motion.
Dizziness – Losing one’s balance while feeling unsteady and lightheaded. May lead to fainting.
Disequilibrium – Lack of mental and emotional balance.
Faintness – A temporary condition in which one is likely to become unconscious and fall.
Headache – A sharp or dull persistent pain in the head.
Hyperreflexia – A not normal (abnormal) and involuntary increased response in the tissues connecting the bones to the muscles.
Light-Headed Feeling – An uncontrolled and usually brief loss of consciousness usually caused by a lack of oxygen to the brain.
Migraine – Recurring severe head pain sometimes accompanied by nausea, vomiting, dizziness, flashes or spots before the eyes and ringing in the ears.
Muscle Contractions Involuntary – A spontaneous and uncontrollable tightening reaction of the muscles caused by electrical impulses from the nervous system.
Muscular Tone Increased – Uncontrolled and exaggerated muscle tension. Muscles are normally partially tensed which is what gives muscle tone.
Paresthesia – Burning, prickly, itchy, or tingling skin with no obvious or understood physical cause.
Restless Legs – A need to move the legs without any apparent reason. Sometimes there is pain, twitching, jerking, cramping, burning or a creepy-crawly sensation associated with the movements. It worsens when a person is inactive and can interrupt sleep so one feels the need to move to gain some relief.
Shaking – Uncontrolled quivering and trembling as if one is cold and chilled.
Sluggishness – Lack of alertness and energy, as well as being slow to respond or perform in life.
Tics – A contraction of a muscle causing a repeated movement not under the control of the person, usually on the face or limbs.
Tremor – A nervous and involuntary vibrating or quivering of the body.
Twitching – Sharp, jerky and spastic motion, sometimes with sharp sudden pain.
Vertigo – A sensation of dizziness with disorientation and confusion.
MENTAL AND EMOTIONAL
Aggravated Nervousness – A progressively worsening, irritated, and troubled state of mind.
Agitation – A suddenly violent and forceful emotionally disturbed state of mind.
Amnesia – Long or short term, partial or full memory loss created by emotional or physical shock, severe illness, or a blow to the head where the person was caused pain and became unconscious.
Anxiety Attack – Sudden and intense feelings of fear, terror, and dread, physically creating shortness of breath, sweating, trembling and heart palpitations.
Apathy – Complete lack of concern or interest for things that ordinarily would be regarded as important or would normally cause concern.
Appetite Decreased – Lack of appetite despite the ordinary caloric demands of living, with a resulting unintentional loss of weight.
Appetite Increased – An unusual hunger causing one to overeat.
Auditory Hallucination – Hearing things without the voices or noises being present.
Bruxism – Grinding and clenching teeth while sleeping.
Carbohydrate Craving – A drive or craving to eat foods rich in sugar and starches (sweets, snacks and junk foods) that intensifies as the diet becomes more and more unbalanced due to the unbalancing of the proper nutritional requirements of the body.
Concentration Impaired – Unable to easily focus attention for long periods of time.
Confusion – Inability to think clearly or understand, preventing logical decision making.
Crying (Abnormal) – Unusual fits of weeping for short or long periods of time for no apparent reason.
Depersonalization – A condition in which one has lost a normal sense of personal identity.
Depression – A hopeless feeling of failure, loss and sadness that can deteriorate into thoughts of death. A very common reaction to or side effect of psychoactive drugs.
Disorientation – A loss of sense of direction, place, time or surroundings, as well as mental confusion regarding one’s personal identity.
Dreaming (Abnormal) – Dreaming that leaves a very clear, detailed picture and impression when awake that can last for a long period of time and sometimes be unpleasant.
Emotional Lability – Suddenly breaking out in laughter or crying or doing both without being able to control the outburst of emotion. These episodes are unstable as they are caused by experiences or events that normally would not have this effect on an individual.
Excitability – Uncontrollably responding to stimuli (one’s environment).
Feeling Unreal – The awareness that one has an undesirable emotion like fear but can’t seem to shake off the irrational feeling. For example, feeling like one is going crazy, but rationally knowing that it is not true. Resembles experiencing a bad dream and not being able to wake up.
Forgetfulness – Unable to remember what one ordinarily would remember.
Insomnia – Sleeplessness caused by physical stress, mental stress or stimulants, such as coffee or medications, awake when one would ordinarily be able to fall and remain asleep.
Irritability – An abnormal reaction of being annoyed or disturbed in response to a stimulus in the environment.
Jitteriness – Nervous fidgeting without apparent cause.
Lethargy – Mental and physical sluggishness and apathy (a feeling of hopelessness that “nothing can be done”) which can deteriorate into an unconscious state resembling deep sleep. A numb state of mind.
Libido Decreased – An abnormal loss of sexual energy or desire.
Panic Reaction – A sudden, overpowering, chaotic and confused mental state of terror resulting in doubt-ridden, often accompanied by hyperventilation and extreme anxiety.
Restlessness Aggravated – A constantly worsening troubled state of mind characterized by increased nervousness, inability to relax and quick temper.
Somnolence – Feeling sleepy all the time or having a condition of semi- consciousness.
Suicide Attempt – An unsuccessful deliberate attack on one’s own life with the intention of ending it.
Suicidal Tendency – Most likely will attempt to kill oneself.
Tremulousness Nervous – Very jumpy, shaky, and uneasy, while feeling fearful and timid. The condition is characterized by dread of the future, involuntary quivering, trembling, and feeling distressed and suddenly upset.
Yawning – Involuntary opening of the mouth with deep inhalation of air.
REPRODUCTIVE FEMALE
Breast Neoplasm – A tumor or cancer, of either of the two milk-secreting organs on the chest of a woman.
Menorrhagia – Abnormally heavy menstrual period or a menstrual flow that has continued for an unusually long period of time.
Menstrual Cramps – Painful, involuntary uterus contractions that women experience around the time of their menstrual period, sometimes causing pain in the lower back and thighs.
Menstrual Disorder – A disturbance or derangement in the normal function of a woman’s menstrual period.
Pelvic Inflammation – The reaction of the body to infectious, allergic or chemical irritation, which, in turn, causes tissue irritation, injury, or bacterial infection characterized by pain, redness, swelling, and sometimes loss of function. The reaction usually begins in the uterus and spreads to the fallopian tubes, ovaries and other areas in the hipbone region of the body.
Premenstrual Syndrome – Various physical and mental symptoms commonly experienced by women of childbearing age usually 2 to 7 days before the start of their monthly period. There are over 150 symptoms including eating binges, behavioral changes, moodiness, irritability, fatigue, fluid retention, breast tenderness, headaches, bloating, anxiety and depression. The symptoms cease shortly after the period begins and disappear with menopause.
Spotting Between Menses – Abnormal bleeding between periods. Unusual spotting between menstrual cycles.
RESPIRATORY SYSTEM
Asthma – A disease of the breathing system initiated by an allergic reaction or a chemical, with repeated attacks of coughing, sticky mucus, wheezing, shortness of breath and a tight feeling in the chest. The disease can reach a state where it stops a person from exhaling, leading to unconsciousness and death.
Breath Shortness – Unnatural breathing, using a lot of effort resulting in not having enough air taken in by the body.
Bronchitis – Inflammation of the two main breathing tubes leading from the windpipe to the lungs. The disease is marked by coughing, a low-grade fever, chest pain and hoarseness. It can also be caused by an allergic reaction.
Coughing – A cough is the response to irritation, such as mucus, that causes the muscles to control the breathing process to expel air from the lungs suddenly and noisily to keep the air passages free from the irritating material.
Laryngitis – Inflammation of the voice box characterized by hoarseness, sore throat, and coughing. It can be caused by straining the voice or exposure to infectious, allergic or chemical irritation.
Nasal Congestion – The presence of an abnormal amount of fluid.
Pneumonia Tracheitis – Bacterial infection of the air passageways and lungs that causes redness, swelling and pain in the windpipe. Other symptoms are high fever, chills, pain in the chest, difficulty breathing and coughing with mucus discharge.
Rhinitis – Chemical irritation causing pain, redness and swelling in the mucus membranes of the nose.
Sinus Congestion – The mucus-lined areas of the bones in the face that are thought to help warm and moisten air to the nose. These areas become clogged with excess fluid or become infected.
Sinus Headache – An abnormal amount of fluid in the hollows of the facial bone structure, especially around the nose. This excess fluid creates pressure, causing pain in the head.
Sinusitis – The body reacts to chemical irritation causing redness, swelling and pain in the area of the hollows in the facial bones, especially around the nose.
SKELETAL
Neck/Shoulder Pain – Hurtful sensations of the nerve endings caused by damage to the tissues in the neck and shoulder, signaling danger of disease.
SKIN AND APPENDAGES (SKIN, LEGS AND ARMS)
Acne – Eruptions of the oil glands of the skin, especially on the face, marked by pimples, blackheads, whiteheads, bumps and more severely, by cysts and scarring.
Alopecia – The loss of hair, baldness.
Angioedema – Intense itching and swelling welts on the skin called hives caused by an allergic reaction to internal or external agents. The reaction is common to a food or a drug. Chronic cases can last for a long period of time.
Dermatitis – Generally irritated skin that can be caused by any of a number of irritating conditions, such as parasites, fungus, bacteria, or foreign substances causing an allergic reaction. It is a general inflammation of the skin.
Dry Lips – The lack of normal moisture in the fleshy folds that surround the mouth.
Dry Skin – The lack of normal moisture/oils in the surface layer of the body. The skin is the body’s largest organ.
Epidermal Necrolysis – An abnormal condition in which a large portion of the skin becomes intensely red and peels off like a second-degree burn. Symptoms often include blistering.
Eczema – A severe or continuing skin disease marked by redness, crusting and scaling, with watery blisters and itching. It is often difficult to treat and will sometimes go away only to reappear again.
Folliculitis – Inflammation of a follicle (small body sac), especially hair follicle.
Furunculosis – Skin boils that show up repeatedly.
Lipoma – A tumor of mostly fat cells that is not health endangering.
Pruritus – Extreme itching of often-undamaged skin.
Rash – A skin eruption or discoloration that may or may not be itching, tingling, burning or painful. It may be caused by an allergy, skin irritation or a skin disease.
Skin Nodule – A bulge, knob, swelling or growth in the skin that is a mass of tissue or cells.
RELATED TO THE SENSES
Conjunctivitis – Infection of the membrane that covers the eyeball and lines the eyelid, caused by a virus, allergic reaction or an irritating chemical. It is characterized by redness, a discharge of fluid and itching.
Dry Eyes – Not enough moisture in the eyes.
Earache – Pain in the ear.
Eye Infection – The invasion of the eye tissue by a bacteria, virus, fungus, etc., causing damage to the tissue, with toxicity. Infection spreading in the body progresses into disease.
Eye Irritation – An inflammation of the eye.
Metallic Taste – A range of taste impairment from distorted taste to a complete loss of taste.
Pupils Dilated – Abnormal expansion of the black circular opening in the center of the eye.
Taste Alteration – Abnormal flavor detection in food.
Tinnitus – A buzzing, ringing or whistling sound in one or both ears occurring from the use of certain drugs.
Vision Abnormal – Normal images are seen differently by the viewer than by others.
Vision Blurred – Eyesight is dim or indistinct and hazy in outline or appearance.
Visual Disturbance – Eyesight is interfered with or interrupted. Examples of disturbances are light sensitivity and the inability to easily distinguish colors.
URINARY SYSTEM
Blood in Urine – Blood is present when one empties the liquid waste product of the kidneys through the bladder by urinating in the toilet, turning the water pink to bright red. Or spots of blood are observable in the water after urinating.
Dysuria – Difficult or painful urination.
Kidney Stone – Small hard masses of salt deposits that the kidney forms.
Urinary Frequency – Having to urinate more often than usual or between unusually short time periods.
Urinary Tract Infection – An invasion of bacteria, viruses, fungi, etc., of the system in the body. This starts with the kidneys, which eliminate urine from the body. If the invasion goes unchecked, it can injure tissue and progress into disease.
Urinary Urgency – A sudden compelling urge to urinate, accompanied by discomfort in the bladder.
UROGENITAL (URINARY TR ACT)
Anorgasmia – Failure to experience an orgasm.
Ejaculation Disorder – Dysfunction during orgasm.
Menstrual Disorder – Dysfunction of the discharge during the monthly menstrual cycle.
VIOLENT OR PHYSICALLY DANGEROUS SIDE EFFECTS
Acute Renal Failure – The kidneys stop excreting waste products properly, leading to rapid poisoning (toxicity) in the body.
Anaphylaxis – A violent, sudden, and severe drop in blood pressure caused by a re-exposure to a foreign protein or a second dosage of a drug that may be fatal unless emergency treatment is given right away.
Grand Mal Seizures (or Convulsions) – A recurring sudden, violent and involuntary attack of muscle spasms with a loss of consciousness.
Neuroleptic Malignant Syndrome – A life threatening, rare reaction to an anti-psychotic drug marked by fever, muscular rigidity, changed mental status and dysfunction of the autonomic nervous system.
Pancreatitis – Chemical irritation with redness, swelling and pain in the pancreas where digestive enzymes and hormones are secreted.
QT Prolongation – A very fast heart rhythm disturbance that is too fast for the heart to beat effectively so the blood to the brain falls, causing a sudden loss of consciousness. May cause sudden cardiac arrest.
Rhabdomyolysis – The breakdown and release of muscle fibers into the circulatory system.
Serotonin Syndrome – A disorder brought on by excessive levels of serotonin. Symptoms include euphoria, drowsiness, sustained and rapid eye movement, agitation, reflexes overreacting, rapid muscle contractions, abnormal movements of the foot, clumsiness, feeling drunk and dizzy without any intake of alcohol, jaw muscles contracting and relaxing excessively, muscle twitching, high body temperature, ridged body, rotating mental status – including confusion and excessive happiness – diarrhea and loss of consciousness.
Thrombocytopenia – An abnormal decrease in the number of blood platelets in the circulatory system. A decrease in platelets causes a decrease in the ability of the blood to clot when necessary.
Torsades de Pointes – Unusually rapid heart rhythm starting in the lower heart chambers. If the short bursts of rapid heart rhythm continue for a prolonged period, it can degenerate into a more rapid rhythm and can be fatal.
Chapter 3
Taper Using Supplements
When you taper using the suggested supplements, taper the Prozac the same as suggested in chapter 1.
If you are currently having strong withdrawal before starting this taper method, you must go back up to the last dosage of Prozac where you felt stable. There is no way around this.
Do this while you are waiting for the supplements to arrive. The supplements are found at www.ngscart.com/products/package-c
Neuro Genetic Solutions has created packages for you, so you do not need to order the supplements individually.
The supplements you will need are Maca Supreme, JNK Formula Complete, Omega 3 Supreme, Neuro Day and Neuro Night. It’s advisable that you order an extra 2 bottles of Maca Supreme.
It’s advisable you order an extra 2 bottles of Maca Supreme and 2 extra bottles of Omega 3 Supreme.
How to Take Supplements
Maca Supreme – It is important you start the Maca Supreme exactly as described in this book.
Take 1 capsule at 8am each day.
4 days later take an additional capsule at 12pm noon.
4 days later take 2 capsules at 8am.
4 days later take 2 capsules at 12pm noon.
Your schedule may not allow you to take the Maca Supreme exactly at 8am or at 12pm noon. If that is the case, take as close to these times as possible.
JNK Formula Complete – After you have taken the 4 Maca Supreme capsules as described above for 4 consecutive days, you are ready to start the JNK Formula and the rest of the supplements.
Take 1 JNK Formula capsule with the 8am Maca Supremes. Take a second JNK Formula with the 12pm noon Maca Supremes.
Neuro Day – Take 1 capsule of the Neuro Day at 10am. Take a second Neuro Day at 2pm.
Neuro Night – Take 2 capsules of Neuro Night about 30 minutes before bedtime.
Omega 3 Supreme – To begin, take 1 softgel each time you take a JNK Formula capsule. You may need to adjust the time you take the Omega 3 Supreme once you begin tapering again.
If you tend to have brain zaps start first thing in the morning, take 1 Omega 3 Supreme when you wake up in the morning. The idea is to look for a trend of the start times of a brain zap and take Omega 3 Supreme at least 30 minutes before they tend to start. This might be in the morning or the afternoon.
With the first reducing of an antidepressant, you may need to take 2 of the Omega 3 Supreme at the same time to get rid of the brain zaps. If you had to go back up on the antidepressant dosage to get rid of the brain zaps, start taking 2 softgels in the morning. You need to eliminate the brain zaps before you restart a taper again.
Restarting the Taper
If you have been tapering the medication before starting this withdrawal method, if you have withdrawal side effects that are in the moderate range to extreme withdrawal, go back up to the last dosage of the medication you were taking that did not have these withdrawal side effects.
While you do this, get the supplements.
When the supplements arrive begin taking them as described.
Take all the supplements for 2 full weeks before resuming the taper again. Then follow the chapter on how to reduce the medications.
You continue taking the supplements throughout the taper. You should continue taking the supplements for 30 days after your last dose of the medication.
It is fine to continue taking the supplements for life if you wish. Many people take one or more of the supplements daily to help with anxiety or sleep.
If Starting the Taper for the First Time
Keep taking the medication at the dosage you have been, and start the supplements exactly as described. Once you have taken the supplements for 14 days you should be ready to start reducing the medication.
Before you start to taper have a look at the graphs you have been keeping and look at the side effects you may still have. Have they greatly reduced? If they have not reduced to a minimal point yet, continue the supplements for one more week and then have another look at the graphs.
If they have not greatly reduced at this point it is time for you to send an email to Jim Harper at Jim@theroadback.org and he will help sort out what is happening.
Only reduce the medication every 14 days and only reduce again if you are feeling very well.
Daily Supplement and Medication Schedule
Keep taking the medication at the same time each day throughout the taper.
Do not take a supplement within 1 hour of when you take the medication.
Maca Supreme – 2 capsules at 8am and 2 at 12 noon.
JNK Formula Complete – Take 1 JNK with the 8am Maca Supreme and 1 capsule with the 12 noon Maca Supreme.
Neuro Day – Take 1 capsule at 10am and 1 capsule at 2pm.
Neuro Night – Take 2 capsules 30 minutes before bedtime.
Omega 3 Supreme – If taking an antidepressant, Take 1 softgel with the morning Maca Supreme and the 12 noon Maca Supreme.
Chapter 4
Journal
The journal is used to note major changes during the taper. Each time you reduce the medication make a note of the date and what dosage you dropped from and to what new lower dosage.
Make note of any diet changes.
Make note of any physical activity.
You do not need to go overboard while keeping a journal, but it is imperative you keep track of changes you have made.
Chapter 5
Graph
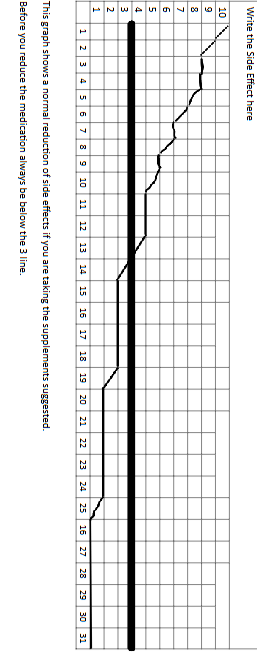
Ideally you will create several graphs. One graph for each major side effect you currently have. Go back to Chapter 2, Prozac Side Effects and make a graph for the major withdrawal side effects you have.
The most common will be anxiety, fatigue, insomnia, body aches and pains.
Get some graph paper and create each graph as provided in the following example.
Write the side effect on the top of the graph, number it from 1-31 and on the left side of the graph you will number from 1-10.
The number 10 should be the most extreme feeling and under number 1 there will be no side effect.
Notice the bolder line at number 3. Any side effect you have should be at a 3 or lower before tapering the Prozac further.
Chapter 6
General Information
This chapter provides general tips and suggestions.
If you have experienced sexual dysfunction, try taking the Maca Supreme as described in the supplement chapter. Give it 30 days and see what changes!
If you are reading this book and are in withdrawal you need to go back up to the last dosage of the medication you felt stable and remain there while you decide your next course of action.
If you are already off the Prozac and still suffering from withdrawal, most likely that withdrawal effect will not stop on its own. Get with your prescribing physician and discuss going back on the medication again. Normally, if you had a dose of the medication, you felt stable during the taper, going back to that dosage will bring relief. I strongly urge you to get the supplements as quickly as possible.
Tapering is one of those things, where doing the same thing over and over and expecting a different result comes to mind. If you have been tapering and suffering withdrawal, unless you change what you have been doing, do not expect a different result.
Slow and steady will win this race.
Prozac Metabolism
Prozac uses liver enzymes to metabolize. Prozac is extensively metabolized by the liver enzyme CYP 2D6. Before going further, I want to detail a bit what these enzymes are, and potential negative and positive.
Roughly one third of the population will metabolize Prozac as the drug is intended to metabolize.
Roughly one third of the population will be a poor metabolizer with Prozac.
The other third will be a rapid metabolizer of Prozac.
Your DNA determines how much enzyme fluid you will have in the CYP 2D6.
This determines how fast or slow the Prozac can move through the liver.
The roughly one third that is an extensive metabolizer with the 2D6 will have a difficult time achieving a therapeutic dosage of the Prozac. A higher dosage of the drug will be needed. This presents additional problems for this group. The drug metabolites do not have a chance to break down and this group will usually develop problems in the kidneys and intestinal tract.
If you are a poor metabolizer of the Prozac, not as much enzyme present, the Prozac may take 48 hours or longer to clear the liver. This can easily lead to an overdose effect. You would need to be taking no more than 10mg daily or possibly the 5mg dosage to avoid the overdose feeling.
If you are taking any other medication that uses the CYP 2D6 to metabolize and you start tapering the Prozac, the other medication metabolism rate will also change. Since the two drug are competing for the same pathway, there is no way the other drug will not also be changing how fast it breaks down in the liver.
These are some reasons you made need to taper Prozac at 5 percent and not 10 percent.
Prozac uses 5 metabolism routes to clear the liver. These are CYP1A2, CYP2C19, CYP2D6, CYP3A.
If you smoke cigarettes, the cigarettes use the CYP1A2 and make any other substance that metabolizes that route speed through. If you stop smoking while taking Prozac, not as much Prozac will clear the body as you are accustomed to, and a slight overdose feeling will occur. The opposite occurs if you start smoking while taking Prozac. The Prozac will clear the body faster and you will feel like you are in withdrawal.
A study was conducted with the antidepressant Cymbalta and it was found smoking will change the metabolism of Cymbalta by 15%. Either up or down.
While you taper, it is important that you not change anything with diet as well. Many people start doing things to get other parts of their life in order when they are about halfway off Prozac. Don’t fall for it. Again, slow and steady wins this race.
The spring and summer months are the time to grill your food on the barbeque. This alters how fast the Prozac will clear the body. Just take notes the next day after you grill and if you do not feel as well, it is best to wait until you are off Prozac.
If you are going to use the supplements suggested, special care has been made to ensure the ingredients of each supplement will not affect the metabolism of Prozac or other medication that use the CYP enzymes for metabolism.
Again, slow and steady wins this race.
During Prozac withdrawal, any and all head symptoms can be handled by taking Omega 3 Supreme.
Stomach upset can normally be handled by drinking a few cups of ginger tea.
If you did not compound the Prozac to get a 10 percent reduction and are just reducing to the next available lower dosage and side effects are too much for you, the thing to try is the supplements suggested.
Make sure to go back up to the last dosage you were feeling stable at before the withdrawal side effects have a chance to really take hold though. Once they do, it is more difficult to taper.
There is a chance your physician will want to prescribe you a different antidepressant if Prozac withdrawal is too much.
I would avoid this completely.
You will be taken off Prozac abruptly and put on a different antidepressant. If you were already having withdrawal from Prozac while tapering the drug, what do you think will happen if you stop Prozac cold turkey?
The best you can hope for is the new antidepressant to mask the Prozac withdrawal, and the new antidepressant does not cause you problems. You are then in a definite fix. Even this program has a difficult time undoing that.
Use Jim Harper for assistance if you need some. Email Jim@theroadback.org
Jim also likes to hear about your successes.
About the Author
In 1999, our founder, Jim Harper, began investigating antidepressants and the cause of their adverse reactions. In 1999, the Internet had two distinct types of websites about psychotropic drugs, those that only stated how bad the drugs were and those sites that only promoted their usage. While others were arguing about the medications, Jim Harper began looking for solutions for withdrawal. Eventually, most every person will reach a point where the physician and patient will want to discontinue the drug and withdrawal assistance needed to be created. In 1999, Jim Harper’s program was the first psychotropic drug withdrawal program.
After 26 years and over 19 million using the program, The Road Back Program is the most widely used drug withdrawal program in the world. The Road Back is a past member of the California Association of Alcoholism & Drug Abuse Counselors (CAADAC).
Jim Harper used the information gathered from his DNA Testing company, Advanced DNA Testing, to advance the program continually over the past decades. After conducting hundreds of DNA test to determine how individuals metabolize psychotropic drugs, evaluating the potential side effects we can all experience due to medications, a basic program was developed. Once DNA testing was completed with hundreds of people regarding their ability to metabolize nutrients and drugs, the program made its next advancement.
Currently, specific supplements are used with The Road Back Program to target genes the drugs activate. The simple process of switching this drug induced activations off again brings relief to the patient during withdrawal.
From all of us at The Road Back – We wish you the best on your journey.
Jim Harper has never used psychotropic medications and is not a recovered addict. Jim has owned a DNA testing company, has been approved by the Los Angeles, CA. courts to be an expert DNA witness and has authored 16 bestselling books about drug withdrawal. One of Jim’s books was used as a textbook at a major university in America in their pharmacology doctoral program.
Jim does understand what you are going through. He has personally answered hundreds of thousands of e-mails over the past 26 years and will answer yours as well and guide you through the withdrawal process.
You will find written in the drug manufacturers description of psychotropic drugs a statement of how to reduce the medication. In 1999, Jim published how to reduce addictive medications and Jim’s approach from 1999 is now recommended by the drug companies. “Reduce the drug slowly and gradually. If side effects become too unbearable, go back up to the last dosage you were doing fine with, get stable once again, and then resume the reduction at a more gradual pace.”
Prozac withdrawal – How to taper Prozac is fully described in How to Taper Psychoactive Medication. The full step by step process in detail. Free assistance is also available if needed.
Prozac Withdrawal Symptoms – What are the symptoms of Prozac withdrawal described as well as how to eliminate Prozac withdrawal symptoms.
Prozac withdrawal – What is the Prozac withdrawal timeline? You will find that in How to Taper Psychoactive Medication. There is a timeline you should follow for a successful Prozac withdrawal.
Prozac withdrawal – Headache is all too common during Prozac withdrawal. Want the solution? It is found in How to Taper Psychoactive Medication.
Prozac withdrawal – Some have anxiety during Prozac withdrawal, and some have fatigue during Prozac withdrawal. How to Taper Psychoactive Medication gives the solutions.
Prozac withdrawal – Nausea during Prozac withdrawal is all too common. It does not need to happen. Read How to Taper Psychoactive Medication for the solution.
Prozac withdrawal – Do you want a list of virtually all Prozac withdrawal side effects? Not only does How to Taper Psychoactive Medication give the Prozac withdrawal side effects but offers solutions.
Prozac withdrawal – Brain zaps caused by Prozac withdrawal can be eliminated quickly. Yes, the solution is in How to Taper Psychotropic Medication.
If you are experiencing brain zaps, electrical jolts in the head, click here
You are likely already in Prozac withdrawal before doing this search. The key to a successful Prozac withdrawal, and being able to stay off Prozac, is to have it be successful. Successful is more than just getting off the Prozac. Successful is, tapering of the Prozac with minimal to no withdrawal. To feel not only stable during withdrawal but to improve your function in life. That is what The Road Back Program is about.
Your first step if you are already in withdrawal. Go back up to the last dosage of Prozac you felt stable at. You may not like this because you feel you will lose the gain you have had in the Prozac withdrawal, but it will save you a lot of time in the short term and long term.
Prozac Withdrawal: A Comprehensive Guide to Symptoms, Duration, and Coping Strategies
Introduction
Prozac (fluoxetine) is a widely prescribed antidepressant medication belonging to the selective serotonin reuptake inhibitor (SSRI) class. It’s commonly used to treat depression, anxiety, and other mental health conditions. While Prozac can be effective in managing symptoms, withdrawal from the medication can be challenging for some individuals. In this comprehensive guide, we’ll explore Prozac withdrawal symptoms, their duration, and coping strategies to help you or a loved one navigate the withdrawal process safely and comfortably.
Section 1: Understanding Prozac Withdrawal
1.1 What is Prozac withdrawal?
1.2 Why does Prozac withdrawal occur?
1.3 Factors influencing Prozac withdrawal.
Section 2: Symptoms of Prozac Withdrawal
2.1 Common Prozac withdrawal symptoms
2.2 Less common and severe withdrawal symptoms
2.3 Protracted withdrawal syndrome
Section 3: Duration of Prozac Withdrawal
3.1 General timeline for Prozac withdrawal
3.2 Factors affecting withdrawal duration
Section 4: Coping Strategies for Prozac Withdrawal
4.1 Medical support and tapering
4.2 Self-care and lifestyle modifications
4.2.1 Sleep and relaxation techniques
4.2.2 Diet and nutrition4.2.3 Exercise and physical activity
4.2.4 Social support and therapy
4.3 Alternative and complementary therapies
4.3.1 Acupuncture
4.3.2 Massage therapy
4.3.3 Herbal remedies
4.3.4 Mindfulness and meditation
Section 5: Preventing Prozac Withdrawal
5.1 Open communication with healthcare providers
5.2 Gradual discontinuation of the medication
5.3 Monitoring for withdrawal symptoms.
Navigating Prozac withdrawal can be a challenging experience, but understanding the process and implementing coping strategies can help minimize discomfort and reduce the risk of complications. By working closely with healthcare providers and practicing self-care, individuals can safely and effectively manage the withdrawal process and transition to a life free from medication dependency.
Section 1: Understanding Prozac Withdrawal
1.1 What is Prozac withdrawal?
Prozac withdrawal, also known as discontinuation syndrome, refers to the collection of symptoms that may arise when an individual stops taking Prozac or significantly reduces the dosage. The symptoms can range from mild to severe, depending on various factors such as the duration of treatment, dosage, and individual differences in metabolism and sensitivity.
1.2 Why does Prozac withdrawal occur?
Prozac works by increasing the levels of serotonin, a neurotransmitter that regulates mood, appetite, and sleep, among other functions. Over time, the brain adjusts to the increased serotonin levels and becomes dependent on the medication to maintain this balance. When the medication is discontinued or reduced, the brain may struggle to readjust, leading to withdrawal symptoms.1.3 Factors influencing Prozac withdrawal.
Several factors can influence the severity and duration of Prozac withdrawal symptoms:
Duration of treatment: Longer treatment periods may result in more significant withdrawal symptoms, as the brain has become more reliant on the medication. Dosage: Higher dosages may lead to more severe withdrawal symptoms, as the brain has become accustomed to higher serotonin levels. Rate of discontinuation: Rapid discontinuation or abrupt cessation of Prozac may cause more intense withdrawal symptoms compared to a gradual tapering of the medication. Individual factors: Genetics, metabolism, and sensitivity to medication can all play a role in the withdrawal experience. People with a history of mental health conditions or previous withdrawal experiences may also be more susceptible to withdrawal symptoms.
Section 2: Symptoms of Prozac Withdrawal2.1 Common Prozac withdrawal symptoms
While the withdrawal experience can vary from person to person, some common symptoms include:
Anxiety
Depression
Irritability
Mood swings
Fatigue
Insomnia
Vivid dreams or nightmares
Headaches
Dizziness
Nausea and vomiting
Flu-like symptoms (chills, fever, body aches) Tremors or muscle spasms
Electric shock sensations (also known as “brain zaps”)
2.2 Less common and severe withdrawal symptoms
Some individuals may experience less common or more severe withdrawal symptoms, such as:
Suicidal thoughts or behaviors
Mania or hypomania
Psychosis
Seizures Intense emotional reactions (e.g., uncontrollable crying, anger, or panic)
Sensory disturbances (e.g., sensitivity to light or sound, visual or auditory hallucinations)2.3 Protracted withdrawal syndrome In some cases, withdrawal symptoms may persist for an extended period, a condition known as protracted withdrawal syndrome (PWS) or post-acute withdrawal syndrome (PAWS). PWS can last for several months or even years and may include symptoms such as:
Persistent anxiety or depression
Cognitive difficulties (e.g., problems with memory, concentration, or decision-making)
Emotional instability or mood swings
Sleep disturbances
Section 3: Duration of Prozac Withdrawal3.1 General timeline for Prozac withdrawal
Prozac has a relatively long half-life compared to other SSRIs, which means it takes longer for the medication to be eliminated from the body. This can result in a more gradual onset of withdrawal symptoms, typically starting within a few days to a week after stopping or reducing the medication. The duration of withdrawal can vary greatly, with symptoms lasting anywhere from a few weeks to several months. In some cases, symptoms may persist for a year or more, particularly in cases of protracted withdrawal syndrome.3.2 Factors affecting withdrawal duration.
As mentioned earlier, factors such as the duration of treatment, dosage, rate of discontinuation, and individual factors can all influence the duration of withdrawal symptoms. To minimize the severity and duration of withdrawal symptoms, it is essential to follow a gradual tapering plan under the supervision of a healthcare professional.
Section 4: Coping Strategies for Prozac Withdrawal4.1 Medical support and tapering
The most effective strategy for managing Prozac withdrawal is to work closely with a healthcare provider who can monitor your progress and provide guidance on tapering the medication. A slow and steady reduction of the dosage over several weeks or months is generally recommended to minimize withdrawal symptoms.4.2 Self-care and lifestyle modifications In addition to medical support, adopting self-care practices and making lifestyle changes can help ease withdrawal symptoms:4.2.1 Sleep and relaxation techniques
Prioritize sleep by maintaining a consistent sleep schedule and creating a comfortable, dark, and quiet sleep environment. Practice relaxation techniques such as deep breathing exercises, progressive muscle relaxation, or guided imagery to reduce stress and anxiety.4.2.2 Diet and nutrition
Eat a balanced diet rich in whole foods, lean proteins, fruits, vegetables, and whole grains. Limit caffeine, sugar, and alcohol, as they can exacerbate withdrawal symptoms. Stay hydrated by drinking plenty of water throughout the day.4.2.3 Exercise and physical activity
Engage in regular physical activity, such as walking, jogging, swimming, or yoga, to help reduce stress, improve mood, and promote better sleep. Aim for at least 30 minutes of moderate exercise most days of the week.4.2.4 Social support and therapy
Reach out to friends, family, or support groups to share your experiences and receive encouragement during the withdrawal process. Consider seeking professional help from a therapist or counselor experienced in managing antidepressant withdrawal.4.3 Alternative and complementary therapies
Some individuals may find relief from withdrawal symptoms through alternative or complementary therapies:
4.3.1 Acupuncture involves the insertion of thin needles into specific points on the body to help balance energy flow and alleviate withdrawal symptoms such as anxiety, depression, and insomnia.4.3.2 Massage therapy
Massage can help relieve muscle tension, reduce stress, and promote relaxation during the withdrawal process.4.3.3 Herbal remedies
Some herbal supplements, such as St. John’s Wort, Valerian root, or passionflower, may help ease withdrawal symptoms. However, it is crucial to consult with a healthcare professional before using any herbal remedies, as they may interact with other medications or have potential side effects.
4.3.4 Mindfulness and meditation
Practicing mindfulness and meditation can help individuals manage stress, anxiety, and depression during withdrawal by fostering self-awareness and promoting relaxation.
Section 5: Preventing Prozac Withdrawal5.1 Open communication with healthcare providers
Maintaining open communication with healthcare providers is essential for preventing or minimizing withdrawal symptoms. Inform your healthcare provider of any concerns or side effects you may be experiencing while taking Prozac.5.2 Gradual discontinuation of the medication
If you and your healthcare provider decide to discontinue Prozac, follow a gradual tapering plan to minimize withdrawal symptoms. Abrupt cessation of the medication can lead to more severe withdrawal symptoms.5.3 Monitoring for withdrawal symptoms
Keep track of any withdrawal symptoms you may experience during the discontinuation process, and share this information with your healthcare provider. They can provide guidance on how to manage these symptoms and adjust your tapering plan if necessary.
Conclusion
Navigating Prozac withdrawal can be a challenging experience, but understanding the process and implementing coping strategies can help minimize discomfort and reduce the risk of complications. By working closely with healthcare providers and practicing self-care, individuals can safely and effectively manage the withdrawal process and transition to a life free from medication dependency. Remember, each person’s withdrawal experience may vary, so it’s essential to listen to your body, communicate openly with your healthcare team, and be patient with the process. With the right support and resources, you can successfully navigate Prozac withdrawal and move forward on your path towards improved mental health and well-being.
Additional Resources
If you or a loved one is facing Prozac withdrawal, it can be helpful to seek out additional resources for support and guidance. Here are a few resources that can help you navigate the withdrawal process:
Mental Health America (MHA): MHA is a national organization dedicated to promoting mental health and offering support for individuals and families affected by mental health conditions. Their website provides information on a variety of topics, including medication withdrawal and support groups. Website: https://www.mhanational.org/National Alliance on Mental Illness (NAMI): NAMI is the largest grassroots mental health organization in the United States, providing advocacy, education, support, and public awareness. They offer various resources, including a helpline, support groups, and educational programs for individuals and families dealing with mental health issues. Website: https://www.nami.org/Anxiety and Depression Association of America (ADAA): ADAA is an international nonprofit organization dedicated to the prevention, treatment, and cure of anxiety, depression, and related disorders. Their website offers resources, including articles, videos, and a directory of mental health professionals, to help individuals and families manage anxiety and depression. Website: https://adaa.org/SAMHSA’s National Helpline: The Substance Abuse and Mental Health Services Administration (SAMHSA) provides a free, confidential helpline for individuals and families facing mental health and substance use disorders. They offer information and referrals to treatment, support groups, and community-based organizations. Helpline: 1-800-662-HELP (1-800-662-4357) Website: https://www.samhsa.gov/find-help/national-helplineOnline support forums: Online forums can offer peer support and a sense of community for individuals going through Prozac withdrawal. Some popular forums include Surviving Antidepressants (https://www.survivingantidepressants.org/) and The Withdrawal Project (https://withdrawal.theinnercompass.org/). Remember, it’s essential to consult with a healthcare professional before making any decisions regarding your medication or treatment plan. These resources are intended to supplement, not replace, professional medical advice and support.
Common Questions and Answers about Prozac WithdrawalQ1: Can I stop taking Prozac cold turkey?
A: Stopping Prozac cold turkey is not recommended, as it can lead to severe withdrawal symptoms. It is crucial to consult with a healthcare professional and follow a gradual tapering plan to minimize withdrawal symptoms and safely discontinue the medication.
Q2: How long do Prozac withdrawal symptoms last?
A: The duration of Prozac withdrawal symptoms can vary greatly, ranging from a few weeks to several months or even longer. Factors such as the duration of treatment, dosage, rate of discontinuation, and individual factors can all influence the severity and duration of withdrawal symptoms.
Q3: Are there any specific steps I should follow when tapering off Prozac?
A: It is essential to work closely with a healthcare professional when tapering off Prozac. They can help develop a personalized tapering plan that gradually reduces the dosage over several weeks or months. This gradual approach can help minimize withdrawal symptoms and ensure a safer discontinuation process.
Q4: Can Prozac withdrawal cause weight gain or weight loss?
A: Changes in weight may occur during Prozac withdrawal, although the specific effects can vary from person to person. Some individuals may experience weight gain due to changes in appetite or increased cravings, while others may experience weight loss due to nausea or a reduced appetite. It’s essential to maintain a balanced diet and engage in regular physical activity to manage weight changes during withdrawal.
Q5: Is it possible to experience withdrawal symptoms even if I’m tapering off Prozac slowly?
A: Yes, it is possible to experience withdrawal symptoms even if you are tapering off Prozac slowly. However, a gradual tapering process can help minimize the severity and duration of withdrawal symptoms. If you experience significant withdrawal symptoms during the tapering process, consult with your healthcare provider for guidance on managing these symptoms and adjusting your tapering plan if necessary.
Q6: Can I use over-the-counter medications to manage withdrawal symptoms?
A: Some over-the-counter medications, such as pain relievers or antacids, may help manage specific withdrawal symptoms like headaches or nausea. However, it’s essential to consult with a healthcare professional before using any over-the-counter medications during withdrawal, as they may interact with other medications or have potential side effects.
Q7: What should I do if I experience severe withdrawal symptoms or feel overwhelmed during the withdrawal process?
A: If you experience severe withdrawal symptoms or feel overwhelmed during the withdrawal process, it is crucial to seek help from a healthcare professional immediately. They can provide guidance on managing these symptoms and adjusting your tapering plan if necessary. In some cases, they may recommend additional support, such as therapy, counseling, or alternative treatments, to help you navigate the withdrawal process.
Q8: Can Prozac withdrawal cause permanent damage?
A: In most cases, Prozac withdrawal symptoms are temporary and resolve over time. However, some individuals may experience protracted withdrawal syndrome (PWS), which can persist for several months or even years. While PWS can be challenging to manage, it does not typically cause permanent damage. Working closely with a healthcare professional and implementing coping strategies can help manage PWS and promote recovery.
Q9: Are there any natural remedies that can help with Prozac withdrawal?
A: Some natural remedies, such as herbal supplements or alternative therapies like acupuncture and massage, may help alleviate withdrawal symptoms. However, it’s essential to consult with a healthcare professional before using any natural remedies, as they may interact with other medications or have potential side effects.
Q10: Is it possible to avoid Prozac withdrawal symptoms altogether?
A: It may not be possible to avoid Prozac withdrawal symptoms entirely, but their severity and duration can be minimized through proper management. Following a gradual tapering plan under the supervision of a healthcare professional, practicing self-care, and implementing coping strategies can help reduce the intensity of withdrawal symptoms and make the process more manageable.
Q11: Can I switch to another antidepressant to help with Prozac withdrawal?
A: In some cases, a healthcare professional may recommend switching to another antidepressant to help manage withdrawal symptoms or address ongoing mental health concerns. This decision should be made in consultation with your healthcare provider, who can determine the most appropriate course of action based on your individual needs and circumstances.
Q12: Can I become addicted to Prozac?
A: Prozac is not considered an addictive substance. However, long-term use can lead to physical dependence, which is why withdrawal symptoms can occur when discontinuing the medication. It’s important to follow your healthcare provider’s recommendations for tapering off Prozac to minimize withdrawal symptoms and avoid potential complications.
Q13: Can Prozac withdrawal cause suicidal thoughts or behaviors?
A: In some cases, Prozac withdrawal may lead to an increase in suicidal thoughts or behaviors, particularly in individuals with a history of depression or other mental health conditions. It is crucial to monitor your mood and mental health during the withdrawal process and seek help from a healthcare professional if you experience suicidal thoughts or concerns about your safety.
Q14: How can I find support from others going through Prozac withdrawal?
A: Support from others going through Prozac withdrawal can be found in various ways, such as online forums, support groups, or therapy sessions. Some popular online forums include Surviving Antidepressants and The Withdrawal Project. Additionally, organizations like NAMI and MHA can help connect you with local support groups and resources.
Q15: Will I need to take another medication after I discontinue Prozac?
A: Whether or not you’ll need to take another medication after discontinuing Prozac depends on your individual circumstances and the reason for taking the medication in the first place. Some individuals may find relief from their symptoms through alternative treatments or lifestyle changes, while others may require ongoing medication management. Consult with your healthcare provider to determine the most appropriate course of action for your needs.
Tips for Talking to Your Healthcare Provider about Prozac Withdrawal
When discussing Prozac withdrawal with your healthcare provider, it’s important to be open, honest, and prepared with the necessary information to ensure a productive conversation. Here are some tips to help guide your discussion:
Write down your concerns and questions: Before meeting with your healthcare provider, make a list of your concerns and any questions you have about Prozac withdrawal. This will help ensure you address all your concerns during the appointment and prevent you from forgetting any important details.
Provide a thorough medical history: Your healthcare provider will need a complete understanding of your medical history to provide the best possible guidance for managing Prozac withdrawal. Be prepared to discuss your previous and current medications, any side effects you’ve experienced, and any other medical conditions or treatments you’ve undergone.
Describe your symptoms: If you’re already experiencing withdrawal symptoms, be as specific as possible when describing them to your healthcare provider. Include information on when the symptoms started, their severity, and any patterns or triggers you’ve noticed.
Discuss your goals: Clearly communicate your goals for discontinuing Prozac and any concerns you have about the process. This will help your healthcare provider understand your needs and create a personalized plan to help you achieve your goals.
Ask about alternative treatments: If you’re interested in alternative treatments or therapies to help manage withdrawal symptoms or address ongoing mental health concerns, ask your healthcare provider for recommendations. They can provide guidance on the safety and efficacy of various treatment options.
Inquire about tapering plans: Your healthcare provider will likely recommend a gradual tapering plan to minimize withdrawal symptoms. Be sure to ask about the specifics of this plan, such as the rate of dosage reduction, the expected duration of the tapering process, and any potential adjustments that may be needed based on your individual circumstances.
Request resources: Ask your healthcare provider for resources to help you better understand Prozac withdrawal and manage the process, such as educational materials, support group information, or referrals to mental health professionals.
Discuss monitoring and follow-up: Talk to your healthcare provider about the best way to monitor your progress and manage any withdrawal symptoms that may arise during the tapering process. This may include regular check-ins, follow-up appointments, or additional support from mental health professionals.
Be open to adjustments: Understand that your tapering plan may need to be adjusted based on your individual experience with withdrawal symptoms. Be open to making changes as needed and maintain ongoing communication with your healthcare provider to ensure the best possible outcome.
Be patient: Prozac withdrawal can be a challenging process, and it’s essential to be patient with yourself and your healthcare provider as you work together to manage the symptoms and safely discontinue the medication. Keep in mind that the process may take longer than expected, and it’s important to prioritize your well-being and mental health throughout the journey.
By following these tips and maintaining open communication with your healthcare provider, you can work together to develop a personalized plan for managing Prozac withdrawal and ensuring a safe, successful transition to a medication-free life or an alternative treatment plan.
Prozac Withdrawal Timeline: What to Expect
When discontinuing Prozac, it’s essential to understand the withdrawal timeline to help you prepare for the process and better manage any symptoms that may arise. Keep in mind that individual experiences can vary, and the following timeline is only intended as a general guideline.
Weeks 1-2:During the first two weeks of tapering off Prozac, you may begin to experience mild withdrawal symptoms. These can include:
Headaches
Dizziness
Fatigue
Nausea
It’s important to maintain open communication with your healthcare provider during this time and report any symptoms you’re experiencing.
Weeks 3-4:As you continue to taper your Prozac dosage, you may experience an increase in withdrawal symptoms. Some common symptoms during this stage can include:
Anxiety
Irritability
Mood swings
Sleep disturbances (insomnia or vivid dreams)
Your healthcare provider may recommend adjusting your tapering plan or implementing coping strategies to help manage these symptoms.
Weeks 5-8:During this stage, you may continue to experience withdrawal symptoms, although their severity may begin to lessen. It’s crucial to stay in contact with your healthcare provider and monitor your progress. Symptoms during this time may include:
Brain zaps (a sensation of electric shocks in the brain)
Decreased appetite
Weight changes
Difficulty concentrating
Ongoing communication with your healthcare provider can help ensure that any adjustments to your tapering plan are made as needed.
Weeks 9-12: As you approach the end of your tapering plan, withdrawal symptoms may continue to lessen in severity. You may still experience lingering symptoms such as:
Fatigue
Anxiety
Mood swings
Sleep disturbances
It’s essential to maintain self-care practices and implement coping strategies during this time to help manage any lingering symptoms.
Weeks 12+:For some individuals, withdrawal symptoms may persist beyond the 12-week mark. This is known as protracted withdrawal syndrome (PWS) and can include symptoms such as:
Anxiety
Depression
Insomnia
Fatigue
If you’re experiencing PWS, it’s important to consult with your healthcare provider for guidance on managing these symptoms and to consider seeking additional support from a mental health professional or support group.
Remember, this withdrawal timeline is only a general guideline, and individual experiences can vary significantly. Factors such as the duration of treatment, dosage, rate of discontinuation, and individual factors can all influence the severity and duration of withdrawal symptoms. By working closely with your healthcare provider and implementing coping strategies, you can better navigate the Prozac withdrawal process and prioritize your mental health and well-being.
Prozac Withdrawal Success Stories: Finding Hope and Inspiration
Hearing about the experiences of others who have successfully navigated Prozac withdrawal can provide hope, inspiration, and valuable insights for those facing the same journey. Here are three success stories from individuals who have managed Prozac withdrawal and regained control of their mental health.
Sarah’s Story:
Sarah began taking Prozac to help manage her anxiety and depression. After several years, she felt ready to discontinue the medication and explore alternative treatments. With her healthcare provider’s guidance, she began a gradual tapering plan and experienced withdrawal symptoms like dizziness, brain zaps, and mood swings.
To manage these symptoms, Sarah prioritized self-care practices, such as regular exercise, a healthy diet, and meditation. She also attended therapy sessions and joined a support group to connect with others going through similar experiences. Over time, Sarah’s withdrawal symptoms subsided, and she successfully discontinued Prozac. Today, she continues to manage her mental health through therapy, self-care, and a strong support network.
David’s Story:
David was prescribed Prozac to help manage his symptoms of depression. After a few years of treatment, he decided, along with his healthcare provider, to discontinue the medication. He followed a personalized tapering plan and experienced withdrawal symptoms, including irritability, sleep disturbances, and headaches.
To cope with these symptoms, David focused on maintaining a regular sleep schedule, engaging in stress-relief activities like yoga, and seeking support from friends and family. He also found solace in online forums where he connected with others going through Prozac withdrawal. Over time, David’s withdrawal symptoms lessened, and he successfully discontinued the medication. Today, he uses a combination of lifestyle changes and therapy to manage his depression.
Emily’s Story:
Emily began taking Prozac to manage her anxiety disorder. After several years of treatment, she felt stable enough to discontinue the medication and explore other ways to manage her anxiety. With her healthcare provider’s support, she developed a tapering plan and experienced withdrawal symptoms such as nausea, dizziness, and increased anxiety.
To manage her symptoms, Emily incorporated relaxation techniques like deep breathing exercises and progressive muscle relaxation into her daily routine. She also began attending therapy sessions to address the root causes of her anxiety and develop healthy coping strategies. Over time, Emily’s withdrawal symptoms subsided, and she successfully discontinued Prozac. Today, she manages her anxiety through a combination of therapy, relaxation techniques, and a supportive network of friends and family.
These success stories demonstrate that it is possible to navigate Prozac withdrawal and regain control of one’s mental health. By working closely with a healthcare provider, implementing coping strategies, and seeking support, individuals can successfully discontinue Prozac and move forward on their journey towards improved mental health and well-being.
Managing Prozac Withdrawal: Coping Strategies and Self-Care Tips
Navigating Prozac withdrawal can be challenging, but implementing coping strategies and prioritizing self-care can help you manage symptoms more effectively. Here are some tips for coping with Prozac withdrawal and maintaining your mental health during the process:
Develop a strong support network: Reach out to friends, family, or support groups to share your experiences and seek encouragement. Connecting with others going through similar situations can help you feel less alone and provide valuable insights and advice.
Practice relaxation techniques: Incorporate relaxation techniques, such as deep breathing exercises, progressive muscle relaxation, or mindfulness meditation, into your daily routine to help manage stress and anxiety.
Prioritize sleep: Maintain a regular sleep schedule and create a sleep-friendly environment to help manage sleep disturbances associated with withdrawal. Avoid caffeine and electronics before bedtime and consider incorporating relaxation techniques into your bedtime routine.
Maintain a balanced diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help support your overall well-being during withdrawal. Be mindful of your caffeine and sugar intake, as these can exacerbate withdrawal symptoms like anxiety and mood swings.
1. “Top antidepressant drugs in the United States based on prescriptions dispensed in 2011-2012” Statista Pharmaceutical Products and Market Report [cited 2022 July 27]
2. Hillhouse TM, Porter JH. A brief history of the development of antidepressant drugs: from monoamines to glutamate. Exp Clin Psychopharmacol. 2015;23(1):1-21. doi:10.1037/a0038550 [cited 2022 July 27]
3. Van Voorhees BW, Smith S, Ewigman B. Treat depressed teens with medication and psychotherapy. J Fam Pract. 2008;57(11):735-9a. [cited 2022 July 27]
4. National Center for Health Statistics, Therapeutic Drug Use [cited 2022 July 27]
5. Stevens DL. Chronic fatigue. West J Med. 2001;175(5):315-319. doi:10.1136/ewjm.175.5.315 [cited 2022 July 27]
6. Grandjean P. Developmental fluoride neurotoxicity: an updated review. Environ Health. 2019 Dec 19;18(1):110. doi: 10.1186/s12940-019-0551-x. PMID: 31856837; PMCID: PMC6923889. [cited 2022 July 27]
7. FDA label Prozac (fluoxetine hydrochloride) 1987 [cited 2022 July 27]
8. Evans EA, Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil. 2014 Aug 14;5:107-20. doi: 10.2147/SAR.S37917. PMID: 25187753; PMCID: PMC4140701. [cited 2022 July 27]
9. Wilson E, Lader M. A review of the management of antidepressant discontinuation symptoms. Ther Adv Psychopharmacol. 2015;5(6):357-368. doi:10.1177/2045125315612334 [cited 2022 July 27]
10. Henssler J, Heinz A, Brandt L, Bschor T. Antidepressant Withdrawal and Rebound Phenomena. Dtsch Arztebl Int. 2019;116(20):355-361. doi:10.3238/arztebl.2019.0355 [cited 2022 July 27]
11. Van Geffen EC, Brugman M, Van Hulten R, Bouvy ML, Egberts AC, Heerdink ER. Patients‘ concerns about and problems experienced with discontinuation of antidepressants. Int J Pharm Pract. 2007; 15:291–293. [cited 2022 July 27]
12. Offidani E, Guidi J, Tomba E, Fava GA. Efficacy and tolerability of benzodiazepines versus antidepressants in anxiety disorders: a systematic review and meta-analysis. Psychother Psychosom. 2013;82(6):355-62. doi: 10.1159/000353198. Epub 2013 Sep 20. PMID: 24061211. [cited 2022 July 27]
13. Black K, Shea C, Dursun S, Kutcher S. Selective serotonin reuptake inhibitor discontinuation syndrome: proposed diagnostic criteria. J Psychiatry Neurosci. 2000 May;25(3):255-61. PMID: 10863885; PMCID: PMC1407715. [cited 2022 July 27]
14. Lane RM. SSRI-induced extrapyramidal side-effects and akathisia: implications for treatment. J Psychopharmacol. 1998;12(2):192-214. doi: 10.1177/026988119801200212. PMID: 9694033.[cited 2022 July 27]
15. Lacasse JR, “Serotonin and Depression: A Disconnect between the Advertisements and the Scientific Literature.” PLOS Medicine 2005 Dec; 2(12): e392 [cited 2022 July 27]
16. Danborg PB, Valdersdorf M, Gøtzsche PC. Long-term harms from previous use of selective serotonin reuptake inhibitors: A systematic review. Int J Risk Saf Med. 2019;30(2):59-71. doi: 10.3233/JRS-180046. PMID: 30714974; PMCID: PMC6839490. [cited 2022 July 27]
17. Kirsch I. Antidepressants and the Placebo Effect. Z Psychol. 2014;222(3):128-134. doi:10.1027/2151-2604/a000176 [cited 2022 July 27]
18. Fan KY, Liu HC. Delirium Associated With Fluoxetine Discontinuation: A Case Report. Clin Neuropharmacol. 2017 May/Jun;40(3):152-153. doi: 10.1097/WNF.0000000000000214. PMID: 28452902. [cited 2022 July 27]
19. Wilson E, Lader M. A review of the management of antidepressant discontinuation symptoms. Ther Adv Psychopharmacol. 2015 Dec;5(6):357-68. doi: 10.1177/2045125315612334. PMID: 26834969; PMCID: PMC4722507. [cited 2022 July 27]
20. US Dept of Health and Human Services, Antidepressant use in children, adolescents, and adults. published online Jan 11, 2017 [cited 2022 July 27]
21. Sharma T, Guski LS, Freund N, Gøtzsche PC. Suicidality and aggression during antidepressant treatment: systematic review and meta-analyses based on clinical study reports. BMJ 2016;352:i65. [cited 2022 July 27]
22. Bielefeldt AØ, Danborg PB, Gøtzsche PC. Precursors to suicidality and violence on antidepressants: systematic review of trials in adult healthy volunteers. J R Soc Med 2016;109:381-392. [cited 2022 July 27]
23. Molero Y, Lichtenstein P, Zetterqvist J, Gumpert CH, Fazel S. Selective Serotonin Reuptake Inhibitors and Violent Crime: A Cohort Study. PLoS Med. 2015;12(9):e1001875. Published 2015 Sep 15. doi:10.1371/journal.pmed.1001875 [cited 2022 July 27]
24. Lagerberg T, Fazel S, Molero Y, et al. Associations between selective serotonin reuptake inhibitors and violent crime in adolescents, young, and older adults – a Swedish register-based study. Eur Neuropsychopharmacol. 2020;36:1-9. doi:10.1016/j.euroneuro.2020.03.024 [cited 2022 July 27]
25. Moore TJ, Glenmullen J, Furberg CD. Prescription drugs associated with reports of violence towards others. PLoS One. 2010 Dec 15;5(12):e15337. doi: 10.1371/journal.pone.0015337. PMID: 21179515; PMCID: PMC3002271. [cited 2022 July 27]
26. Pesce N, “Anti-anxiety medication prescriptions have spiked 34% during the coronovirrus pandemic.” May 26 2020 Marketwatch Report [cited 2022 July 27]
27. Miron O, Yu KH, Wilf-Miron R, Kohane IS. Suicide Rates Among Adolescents and Young Adults in the United States, 2000-2017. JAMA. 2019;321(23):2362-2364. doi:10.1001/jama.2019.5054 [cited 2022 July 27]
28. Zajecka J, Tracy KA, Mitchell S. Discontinuation symptoms after treatment with serotonin reuptake inhibitors: a literature review. J Clin Psychiatry. 1997 Jul;58(7):291-7. doi: 10.4088/jcp.v58n0702. PMID: 9269249.[cited 2022 July 27]
29. Haddad P. Newer antidepressants and the discontinuation syndrome. J Clin Psychiatry. 1997;58 Suppl 7:17-21; discussion 22. PMID: 9219489. [cited 2022 July 27]
30. Akagi H, Kumar TM. Lesson of the week: Akathisia: overlooked at a cost. BMJ. 2002;324(7352):1506-1507. doi:10.1136/bmj.324.7352.1506 [cited 2022 July 27]
31. Brambilla P, Cipriani A, Hotopf M, Barbui C. Side-effect profile of fluoxetine in comparison with other SSRIs, tricyclic and newer antidepressants: a meta-analysis of clinical trial data. Pharmacopsychiatry. 2005 Mar;38(2):69-77. doi: 10.1055/s-2005-837806. PMID: 15744630. [cited 2022 July 27]
32. Voican CS, Corruble E, Naveau S, Perlemuter G. Antidepressant-induced liver injury: a review for clinicians. Am J Psychiatry. 2014 Apr;171(4):404-15. doi: 10.1176/appi.ajp.2013.13050709. PMID: 24362450. [cited 2022 July 27]
33. De Picker L, Van Den Eede F, Dumont G, Moorkens G, Sabbe BG. Antidepressants and the risk of hyponatremia: a class-by-class review of literature. Psychosomatics. 2014 Nov-Dec;55(6):536-47. doi: 10.1016/j.psym.2014.01.010. Epub 2014 Apr 21. PMID: 25262043. [cited 2022 July 27]
34. Jonsson GW, Moosa MY, Jeenah FY. Toxic epidermal necrolysis and fluoxetine: a case report. J Clin Psychopharmacol. 2008 Feb;28(1):93-5. doi: 10.1097/jcp.0b013e3181604015. PMID: 18204349. [cited 2022 July 27]
35. Bloechliger M, Ceschi A, Rüegg S, Kupferschmidt H, Kraehenbuehl S, Jick SS, Meier CR, Bodmer M. Risk of Seizures Associated with Antidepressant Use in Patients with Depressive Disorder: Follow-up Study with a Nested Case-Control Analysis Using the Clinical Practice Research Datalink. Drug Saf. 2016 Apr;39(4):307-21. doi: 10.1007/s40264-015-0363-z. PMID: 26650063. [cited 2022 July 27]
36. Laporte S, Chapelle C, Caillet P, Beyens MN, Bellet F, Delavenne X, Mismetti P, Bertoletti L. Bleeding risk under selective serotonin reuptake inhibitor (SSRI) antidepressants: A meta-analysis of observational studies. Pharmacol Res. 2017 Apr;118:19-32. doi: 10.1016/j.phrs.2016.08.017. Epub 2016 Aug 10. PMID: 27521835. [cited 2022 July 27]
37. Amsterdam JD, Garcia-España F, Goodman D, Hooper M, Hornig-Rohan M. Breast enlargement during chronic antidepressant therapy. J Affect Disord. 1997 Nov;46(2):151-6. doi: 10.1016/s0165-0327(97)00086-4. PMID: 9479619. [cited 2022 July 27]
38. Kaufman KR, Podolsky D, Greenman D, Madraswala R. Antidepressant-selective gynecomastia. Ann Pharmacother. 2013 Jan;47(1):e6. doi: 10.1345/aph.1R491. Epub 2013 Jan 16. PMID: 23324513. [cited 2022 July 27]
39. Gerber PE, Lynd LD. Selective serotonin-reuptake inhibitor-induced movement disorders. Ann Pharmacother. 1998 Jun;32(6):692-8. doi: 10.1345/aph.17302. PMID: 9640489. [cited 2022 July 27]
40. Henry C, Sorbara F, Lacoste J, Gindre C, Leboyer M. Antidepressant-induced mania in bipolar patients: identification of risk factors. J Clin Psychiatry. 2001 Apr;62(4):249-55. doi: 10.4088/jcp.v62n0406. PMID: 11379838.[cited 2022 July 27]
41. Machado-Vieira R, Baumann J, Wheeler-Castillo C, et al. The Timing of Antidepressant Effects: A Comparison of Diverse Pharmacological and Somatic Treatments. Pharmaceuticals (Basel). 2010;3(1):19-41. Published 2010 Jan 6. doi:10.3390/ph3010019 [cited 2022 July 27]
42. Gomez R, Huber J, Tombini G, Barros HM. Acute effect of different antidepressants on glycemia in diabetic and non-diabetic rats. Braz J Med Biol Res. 2001 Jan;34(1):57-64. doi: 10.1590/s0100-879×2001000100007. PMID: 11151029. [cited 2023 May 17]
43. Desimone ME, Weinstock RS. Hypoglycemia. [Updated 2018 May 5]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279137/ [cited 2023 May 17]
44. Jacques A, Chaaya N, Beecher K, Ali SA, Belmer A, Bartlett S. The impact of sugar consumption on stress driven, emotional and addictive behaviors. Neurosci Biobehav Rev. 2019 Aug;103:178-199. doi: 10.1016/j.neubiorev.2019.05.021. Epub 2019 May 21. PMID: 31125634.[cited 2023 May 17]
45. Brambilla P, Cipriani A, Hotopf M, Barbui C. Side-effect profile of fluoxetine in comparison with other SSRIs, tricyclic and newer antidepressants: a meta-analysis of clinical trial data. Pharmacopsychiatry. 2005 Mar;38(2):69-77. doi: 10.1055/s-2005-837806. PMID: 15744630.[cited 2023 May 17]
46. Schildkrout B. How to Move Beyond the Diagnostic and Statistical Manual of Mental Disorders/International Classification of Diseases. J Nerv Ment Dis. 2016 Oct;204(10):723-727. doi: 10.1097/NMD.0000000000000547. PMID: 27748696. [cited 2022 July 27]
47. Harris E, Eng HY, Kowatch R, Delgado SV, Saldaña SN. Disinhibition as a side effect of treatment with fluvoxamine in pediatric patients with obsessive-compulsive disorder. J Child Adolesc Psychopharmacol. 2010 Aug;20(4):347-53. doi: 10.1089/cap.2009.0126. PMID: 20807074. [cited 2022 July 27]
48. Sarkar S, Varshney M. Yoga and substance use disorders: A narrative review. Asian J Psychiatr. 2017 Feb;25:191-196. doi: 10.1016/j.ajp.2016.10.021. Epub 2016 Nov 5. PMID: 28262148. [cited 2023 Mar 9]
49. Angelopoulou E, Anagnostouli M, Chrousos GP, Bougea A. Massage therapy as a complementary treatment for Parkinson’s disease: A Systematic Literature Review. Complement Ther Med. 2020 Mar;49:102340. doi: 10.1016/j.ctim.2020.102340. Epub 2020 Feb 6. PMID: 32147033. [cited 2023 May 17]
50. Geoffroy PA, Micoulaud Franchi JA, Lopez R, Schroder CM; membres du consensus Mélatonine SFRMS. The use of melatonin in adult psychiatric disorders: Expert recommendations by the French institute of medical research on sleep (SFRMS). Encephale. 2019 Nov;45(5):413-423. doi: 10.1016/j.encep.2019.04.068. Epub 2019 Jun 24. PMID: 31248601. [cited 2023 May 17]
51. Marcus, M. T., & Zgierska, A. (2009). Mindfulness-based therapies for substance use disorders: part 1. Substance abuse, 30(4), 263–265. https://doi.org/10.1080/08897070903250027 [cited 2023 May 17]
52. Firth, J., Gangwisch, J. E., Borisini, A., Wootton, R. E., & Mayer, E. A. (2020). Food and mood: how do diet and nutrition affect mental wellbeing?. BMJ (Clinical research ed.), 369, m2382. https://doi.org/10.1136/bmj.m2382 [cited 2023 May 17]
53. Clapp, M., Aurora, N., Herrera, L., Bhatia, M., Wilen, E., & Wakefield, S. (2017). Gut microbiota’s effect on mental health: The gut-brain axis. Clinics and practice, 7(4), 987. https://doi.org/10.4081/cp.2017.987 [cited 2023 May 17]
54. Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings. Geneva: World Health Organization; 2009. 4, Withdrawal Management. Available from: https://www.ncbi.nlm.nih.gov/books/NBK310652/ [cited 2023 May 17]
55. Oesterle, T. S., Kolla, B., Risma, C. J., Breitinger, S. A., Rakocevic, D. B., Loukianova, L. L., Hall-Flavin, D. K., Gentry, M. T., Rummans, T. A., Chauhan, M., & Gold, M. S. (2020). Substance Use Disorders and Telehealth in the COVID-19 Pandemic Era: A New Outlook. Mayo Clinic proceedings, 95(12), 2709–2718. https://doi.org/10.1016/j.mayocp.2020.10.011 [cited 2023 May 17]
56. Evans EA, Sullivan MA. Abuse and misuse of antidepressants. Subst Abuse Rehabil. 2014 Aug 14;5:107-20. doi: 10.2147/SAR.S37917. PMID: 25187753; PMCID: PMC4140701.[cited 2023 May 17]
57. Chiappini S, Vickers-Smith R, Guirguis A, Corkery JM, Martinotti G, Schifano F. A Focus on Abuse/Misuse and Withdrawal Issues with Selective Serotonin Reuptake Inhibitors (SSRIs): Analysis of Both the European EMA and the US FAERS Pharmacovigilance Databases. Pharmaceuticals (Basel). 2022 May 1;15(5):565. doi: 10.3390/ph15050565. PMID: 35631391; PMCID: PMC9146999.[cited 2023 May 17]